When it comes to diagnosing amyloidosis, a lot of emphasis is placed on doctors and other HCPs being well informed about the condition. That’s true, but what’s also true in rare diseases like amyloidosis, is that the person / patient in front of them needs to be well informed too. In amyloidosis, knowledge is power! Our job is to arm you with the information you need, to be able to advocate for yourself (and/or your loved one), and to be actively involved decisions about your (and / or your loved one’s) health. In the previous article we covered steps 1 and 2 in the path to diagnosis. Here we cover step 3 which involves a little more detective work.
Step 3: Some detective work
Amyloidosis is diagnosed through a combination of medical assessment, laboratory tests, scans, and biopsy. The specifics depend on the type of amyloidosis and which organs are affected. It’s often the case that the doctor(s) reach a diagnosis by the process of ruling out other conditions and types, known as a ‘diagnosis by exclusion’. This is because of the vague nature of many of the early symptoms, and because there are many different types of amyloidosis, and there’s a lot of overlap in terms of which organs are affected or ‘involved’ (see figure below).
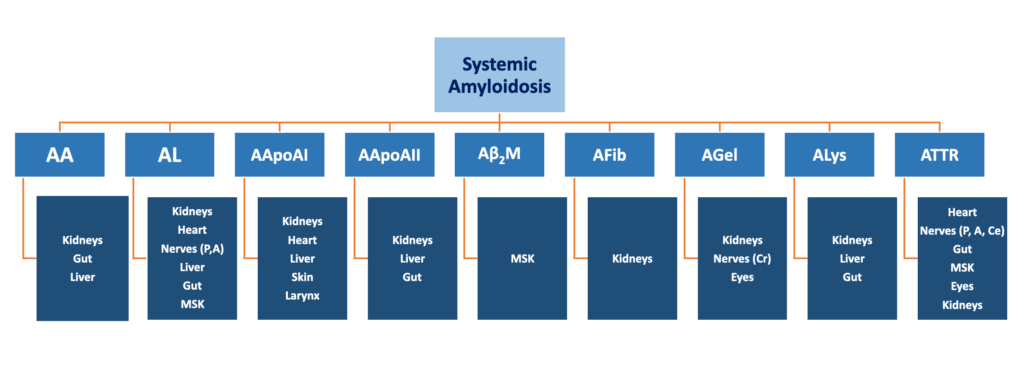
Nerves: P = peripheral; A = autonomic; Cr = cranial; Ce = central)
MSK = musculoskeletal
Tests and investigations
In medicine, tests and investigations are related but distinct concepts.
A test is a specific procedure used to check for a particular condition or measure something. It usually has a defined procedure or protocol that produces a measurable result (e.g., positive/negative, or a number). Some examples are:
- Blood tests, such as a glucose test or a full blood count, (FBC)
- Imaging tests, like MRI, ultrasound, X-ray.

An investigation is a broader process of gathering and analysing clinical information to reach a diagnosis. It may include multiple tests, medical history, physical exam, and other diagnostic methods. For example, someone who is undergoing investigation of chest pain may have an ECG, a blood test for troponins, and a chest X-ray.
The key difference is that:
- A test is a single diagnostic procedure, while an investigation is a broader process that may include multiple tests and assessments
- Tests provide data, while investigations interpret and combine those data to reach a clinical decision
Tests for amyloidosis
These are specific procedures used to detect amyloid deposits, identify the specific type, and assess organ function.
Detecting and typing
1. Biopsy
Biopsy is an invasive procedure that is commonly (but not always) performed to diagnose amyloidosis. A needle is used to take a small sample from an organ or other soft tissue, and this is sent to the lab for testing. A dye called Congo red is applied to the tissue in a process called ‘staining’; amyloid deposits in the tissue absorb the stain and when examined under a microscope, they’ll show up as red specks initially; they then change colour when looked at with a specific type of lens/filter (a phenomenon called ‘birefringence’).
Once amyloid deposits have been found in the biopsy, the type must be determined. This is done using a lab technique called immunohistochemistry, which uses antibodies to identify proteins in tissue samples. Antibodies are protein detectors – they stick (or ‘bind’) to specific proteins, making them visible under a microscope. To determine the type of amyloidosis, the lab technicians will use antibodies designed to bind to specific amyloidosis precursor proteins.

2. Imaging (scanning)
Biopsy is an invasive procedure and, in some cases, cannot be performed quickly, easily or safely.
The development of non-invasive methods of detecting and measuring amyloid deposits has been a game-changer, particularly for those with cardiac amyloidosis. Before innovations in nuclear imaging (scintigraphy) and cardiac magnetic resonance (CMR) imaging, people with suspected cardiac amyloidosis would have to undergo a biopsy of the heart to confirm amyloid deposits and type. However, many patients were too poorly to have the procedure and sadly died without a diagnosis. These days DPD (or PYP or HMDP) scintigraphy is widely available and relatively inexpensive, enabling many with cardiac ATTR amyloidosis to get diagnosed quickly. CMR imaging techniques have also evolved to enable not only quick diagnosis but also changes in the heart over time. The latter means that doctors can now monitor whether your heart is getting better with treatment!!
SAP scintigraphy is another type of nuclear scan and has been available for several decades in the UK and the Netherlands. This scan was invented at the National Amyloidosis Centre in London and was the first ever non-invasive diagnostic and monitoring test in amyloidosis. The SAP scan is different from the DPD scan in that it is used to detect and measure amyloid deposits in all other all other organs, apart from the heart.
Assessing organ function
- Blood tests
- Full blood count (FBC) — assesses for anaemia or other abnormalities in blood cell counts
- Biochemistry panel — provides information on how the kidneys and liver are functioning; these organs are affected in several types of amyloidosis
- Cardiac biomarkers — levels of proteins called NT-proBNP and troponins are elevated in cardiac amyloidosis
- Serum protein electrophoresis (sPEP) — detects abnormal proteins called monoclonal proteins (or ‘M proteins’) that are present in AL amyloidosis
- Serum immunofixation electrophoresis (sIFE) — a more sensitive test than sPEP for detecting small amounts of monoclonal proteins in AL. This test is also useful in identifying the specific type of abnormal M protein
- Serum free light chain (sFLC) assay — measures free kappa and lambda light chains; a high level of kappa or lambda, or an abnormal kappa/lambda ratio suggests AL amyloidosis
- Genetic panel — to rule out or confirm a hereditary form of amyloidosis.
- Urine tests
- Urine protein electrophoresis (uPEP) — detects M proteins in the urine of AL patients.
- Urine immunofixation electrophoresis (uIFE) — a more sensitive test for detecting small amounts of monoclonal proteins in AL. This is a very important test for distinguishing cardiac AL from cardiac ATTR amyloidosis.
- 24-hour urine collection — this test involves peeing in a special bottle for a full day(!). The sample is sent to the lab where the amount of protein in the urine (‘proteinuria’) is measured. If this is abnormally high it indicates the kidneys aren’t functioning as they should. The kidneys are the most frequently affected organs in amyloidosis, so many readers will be familiar with the ‘collection’ process.
- Other tests
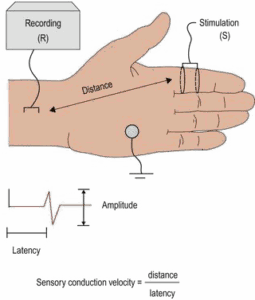
- Nerve conduction studies (NCS) — are performed when nerve involvement is suspected. This test of sensory nerve (the nerves involved in sensations such as touch and temperature) function involves stimulating a nerve at a chosen point, e.g., one of the fingers, and then recording the speed and strength of the stimulus at another point further up the arm. If the speed is slower (‘latency’), and strength (‘amplitude’) is reduced, it means the sensory nerves are affected by the amyloidosis.
- Electromyography (EMG) — the procedure here is like NCS, however, the aim is to test the motor nerves (those involved in movement) and response of the muscle to the stimulus
- Autonomic nerve function tests — the autonomic nerves can be thought of as those controlling the ‘automatic’ bodily functions. These include organs such as the heart, bladder and bowel, as well as sexual function.

- Orthostatic (‘standing up’) response tests — the tilt table test is a commonly performed test that provides reliable and valuable information about autonomic nerve function. You’d be very securely strapped to a movable table, which is then tilted to different angles. Various attached monitoring devices assess how your cardiovascular and nervous systems respond to the change in position. The test mimics how your blood pressure changes when you go from lying to sitting or standing.
- Echocardiogram (Echo) — an ultrasound scan of the heart that can assess how well the heart is pumping and if there are any changes to the structure of the heart, e.g., the thickness of the heart walls and sizes of the different ‘chambers’.
Summary
Getting to a firm diagnosis of amyloidosis and the specific type can involve a lengthy investigative journey due to the need to perform many diagnostic procedures, eliminate other conditions, and conduct tests of organ function. Although it can be frustrating and scary, it’s important to get it right!
Next week: Focus on cardiac amyloidosis – how to GET IT RIGHT!





